In this post, we’ll describe medical imaging workflow as it specifically applies to DXA based bone densitometry. Radiology departments, imaging centers, and hospitals have implemented efficient processes that maximize the volume of patients, along with revenue, and also minimize errors.
This posting assumes modern technology is in place, such as electronic medical records (EMRs), hospital information systems (HIS), radiology information systems (RIS), DICOM for electronic image transfer, and picture archiving systems (PACS). For a reporting system, we’ll assume BoneStation is used. We’ll also assume the EMR, HIS, or RIS provide order entry and results capabilities (where ordering providers view test results).
The following diagram depicts typical workflow, but adapted for DXA based bone densitometry. The workflow can be thought of as an assembly line, where the patients navigate through the process. Often times, patient flow may be tracked throughout the day via the EMR/RIS/HIS.
1) An order is placed (scheduled) for a bone density test. Often times the ordering provider calls the bone density practice to order a test. The order is entered into the EMR/RIS/HIS.
2) Patient arrives for the exam on the scheduled day.
The receptionist may log into the EMR/RIS/HIS and update a patient’s status to “arrived”.
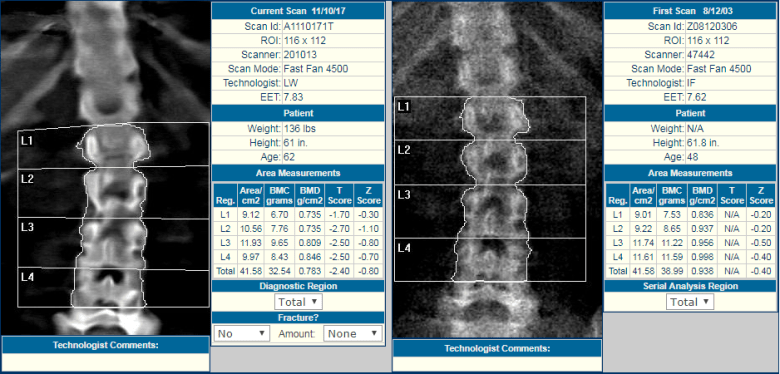
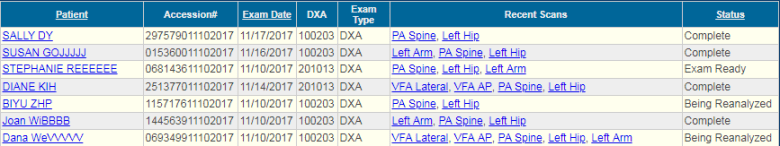
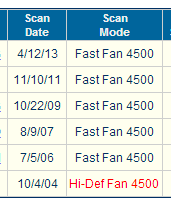
3) A DXA technologist scans the patient on the bone densitometer, analyzes the scans in the DXA software, and transmits the scans, via DICOM, to BoneStation. BoneStation extracts all the quantitative data and the images.
If DICOM Modality Worklist (MWL) is available on the DXA, the tech may pull all the patient info (name, DOB, ethnicity, etc) electronically from the EMR/RIS/HIS into the DXA software. Otherwise the technologist manually enters patient demographics.
The technologist logs on to BoneStation and fills in the patient history questionnaire. FRAX is built into BoneStation, and the questionnaire is filled out there instead of in the DXA software. There are advantages to having questionnaires in BoneStation, which are discussed here.
The technologist may update the patient’s status in the EMR to “complete”.
4) A physician, that is specially trained to read DXA scans, logs into BoneStation and reads the bone density scans. BoneStation automates much of the process of reading scans. The final output is a bone density report. This video demonstrates how easily and quickly reading scans is in BoneStation.
5) BoneStation distributes the report to the EMR/RIS/HIS. BoneStation creates fully formatted reports, with tables, images, and charts. Click here to see some sample reports. Depending on the interface between BoneStation and the EMR, only a text report may be available or the fully formatted report in the EMR.
BoneStation supports a variety of ways to distribute reports, including printing and faxing. This article provides more info about one instance of a BoneStation to Epic interface.
Once the EMR receives the bone density report, the patient’s status is updated to “final”. This may also trigger events related to billing. The process for the patient’s scan is now complete.
6) The ordering provider accesses the report in the EMR/RIS/HIS. Some EMRs may notify the ordering provider that results have been received when the report is received by the EMR/RIS/HIS.
The workflow described here is typical for most hospitals, radiology departments and imaging centers. There are some unique aspects that are specific to DXA. We will go into more detail regarding DXA in a future posting.